Laser therapy has emerged as a promising option for treating fungal infections, particularly those affecting the nails.
Traditional methods, like topical and oral antifungal medications, have their limitations, such as prolonged treatment times and potential side effects.
In contrast, laser treatment offers a non-invasive, effective, and increasingly popular solution.
In this article, we’ll explore how laser treatments work against fungal infections, their effectiveness, the advantages they offer, and who might benefit most from them.
Understanding Fungal Infections and Their Challenges
Fungal infections, such as those affecting nails (onychomycosis), skin (ringworm), and other areas, are caused by fungi that thrive in warm, moist environments.
Once they take hold, these infections can be difficult to eradicate, especially when they penetrate deeper layers of tissue, like under the nail bed.
Traditional treatments, while effective, often require extended use and may cause side effects:
- Topical Treatments: Often used for mild infections, but may have limited effectiveness if the fungus has spread to deeper layers.
- Oral Antifungals: Generally effective, but may come with side effects like liver issues, especially with prolonged use.
Laser therapy offers a different approach by using concentrated light energy to target and kill fungi without the side effects of medications.
Book Your Skin Consultation with Dr. Harmandeep Sidhu
Trusted dermatologist in Chandigarh. Get expert care in skin, hair and lasers at Athena Skin Clinic.

How Laser Therapy Works on Fungal Infections
Laser treatments for fungal infections use specific wavelengths of light to penetrate the skin and nail tissue, targeting the fungi while preserving the surrounding healthy cells.
Lasers produce intense heat that damages fungal cells, disrupting their structure and ultimately leading to their destruction.
This process is both direct and efficient, aiming to eradicate the fungi in a way that traditional treatments often cannot.
Key Mechanisms:
- Heat-Based Destruction: The laser heats fungal cells without affecting other cells, helping to stop the infection’s spread.
- Selective Targeting: Advanced lasers can be tuned to specifically target fungal cells, reducing damage to surrounding tissues.
- Improved Penetration: Laser light can penetrate through nail and skin layers, making it particularly effective for fungal infections under the nail, where topical treatments may fail to reach.
Types of Laser Treatments for Fungal Infections
Different types of lasers are used for fungal infections, each with specific features:
Nd Lasers
- One of the most common lasers used for fungal infections.
- Penetrates deeply into the nail and skin, targeting fungal cells effectively.
- Requires minimal downtime and is generally painless.
CO2 Lasers
- Known for high precision, CO2 lasers may be used for more extensive fungal infections.
- They require careful administration but can be highly effective for tough infections.
Diode Lasers
- Diode lasers offer excellent penetration, especially for toenail fungus.
- Often requires multiple sessions to achieve optimal results.
Each laser type has its own benefits and may be chosen based on the infection severity, patient’s health, and treatment goals.
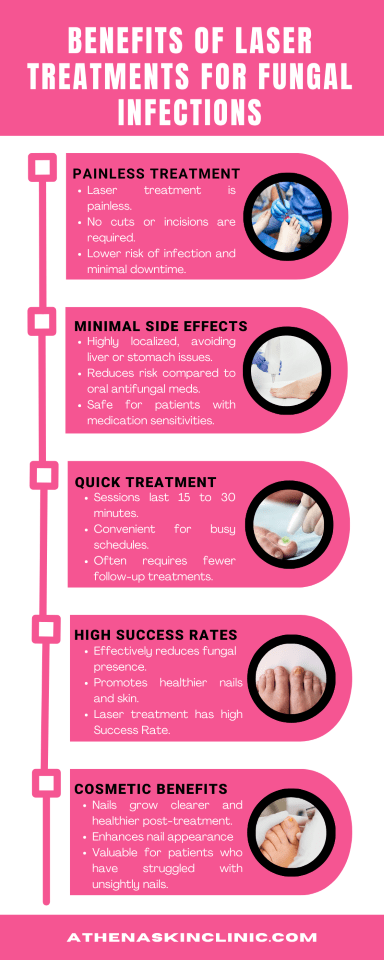
Benefits of Laser Treatments for Fungal Infections
Laser treatments offer several distinct advantages over conventional treatments:
1. Non-Invasive and Painless
Laser therapy is generally painless, with patients only feeling a mild warming or tingling sensation during the session.
Non-invasive, meaning no cuts or incisions, reducing the risk of infection and downtime.
2. Minimal Side Effects
Unlike oral antifungal medications, which may cause liver or gastrointestinal issues, laser therapy is highly localized, resulting in minimal to no side effects.
3. Quick Treatment Time
Sessions typically last between 15 to 30 minutes, making it convenient for busy patients.
Fewer follow-up treatments may be required compared to other methods.
4. High Success Rates
Studies show that laser treatments can significantly reduce fungal presence, leading to healthier nails and skin.
The ability of lasers to penetrate deeply makes them effective for infections that are resistant to other treatments.
5. Cosmetic Benefits
As nails grow out after treatment, they may appear clearer and healthier, enhancing their appearance.
This is especially valuable for patients who have struggled with unsightly nails due to long-term infections.
What to Expect During Laser Treatment for Fungal Infections
Laser treatment for fungal infections is usually performed in a clinical setting by a dermatologist or specialist.
Here’s what patients can generally expect:
Initial Consultation:
The healthcare provider will assess the extent of the infection, discuss health history, and explain the procedure and expected outcomes.
In cases of nail fungus, the infected nail(s) may be trimmed or filed down to allow better laser penetration.
During the Procedure:
The area will be cleaned and prepped.
A handheld laser device will be directed at the infected area, emitting light pulses. Patients may feel warmth but generally report minimal discomfort.
Each session lasts approximately 15–30 minutes, depending on the size and severity of the infection.
Post-Treatment Care:
Minimal to no downtime is needed, and patients can typically resume normal activities right away.
Results may not be visible immediately; as the nail grows out, the treated area will gradually show improvement.
Follow-up sessions may be scheduled based on the infection’s response to treatment.
Who Can Benefit from Laser Therapy?
Laser treatments are suitable for a variety of fungal infections, but they may be especially beneficial for:
- Individuals with Toenail or Fingernail Fungus: This is often one of the hardest infections to treat conventionally, and lasers are highly effective here.
- Those Who Can’t Take Oral Antifungals: Patients with liver disease or sensitivities to oral medications can benefit from this non-invasive alternative.
- People Seeking a Quick, Side-Effect-Free Treatment: Those with busy lifestyles or concerns about medication side effects may find laser treatment ideal.
- Individuals with Recurring Fungal Infections: For those with chronic or stubborn infections, lasers can offer a durable solution.
Effectiveness and Success Rates of Laser Treatment
Laser treatments for fungal infections have shown positive results in clinical studies, with a success rate ranging from 70% to 90% in some cases. The effectiveness often depends on factors such as:
- Severity and Extent of the Infection: Deeper or more extensive infections may require multiple sessions.
- Type of Laser Used: Some lasers have proven more effective for specific fungi or deeper penetration.
- Patient Adherence: Consistent follow-up and good hygiene can increase the chances of long-term success.
Although laser treatment is promising, it’s not always a guaranteed cure. For best results, patients should adhere to recommended follow-up care and maintain good hygiene practices.
Risks and Limitations
While laser treatments are generally safe, they do have some limitations:
- Cost: Laser treatments can be expensive, and are often not covered by insurance as they may be considered cosmetic.
- Multiple Sessions Needed: Some infections may require several treatments, leading to higher costs and more clinic visits.
- Potential Recurrence: As with other treatments, there’s a chance the infection could return if preventive measures aren’t taken.
Tips for Post-Treatment Care to Prevent Recurrence
Laser treatment can effectively eliminate fungal infections, but following these tips can help prevent a recurrence:
- Practice Good Foot and Nail Hygiene: Clean and dry feet thoroughly, especially between toes.
- Wear Breathable Footwear: Opt for shoes that allow air circulation.
- Avoid Walking Barefoot in Public Areas: Wear protective footwear in shared spaces like pools and gyms.
- Change Socks Regularly: Keep feet dry by changing socks if they get sweaty.
- Use Antifungal Powder or Spray: Especially helpful in keeping fungal growth at bay.
Conclusion:
Laser therapy has become a game-changer for managing fungal infections, providing an effective, non-invasive alternative to traditional treatments.
With minimal downtime and fewer side effects, laser treatments can be an ideal option for those seeking a quick, convenient solution.
However, it’s essential to consult with a dermatologist in Chandigarh to determine if this treatment is right for you.
With the right aftercare and preventive steps, laser therapy can help keep fungal infections at bay and restore the health and appearance of your skin and nails.